Orthopedic Specialties
Where’s your pain?
Please click the appropriate body part below to view more information about conditions and procedures.
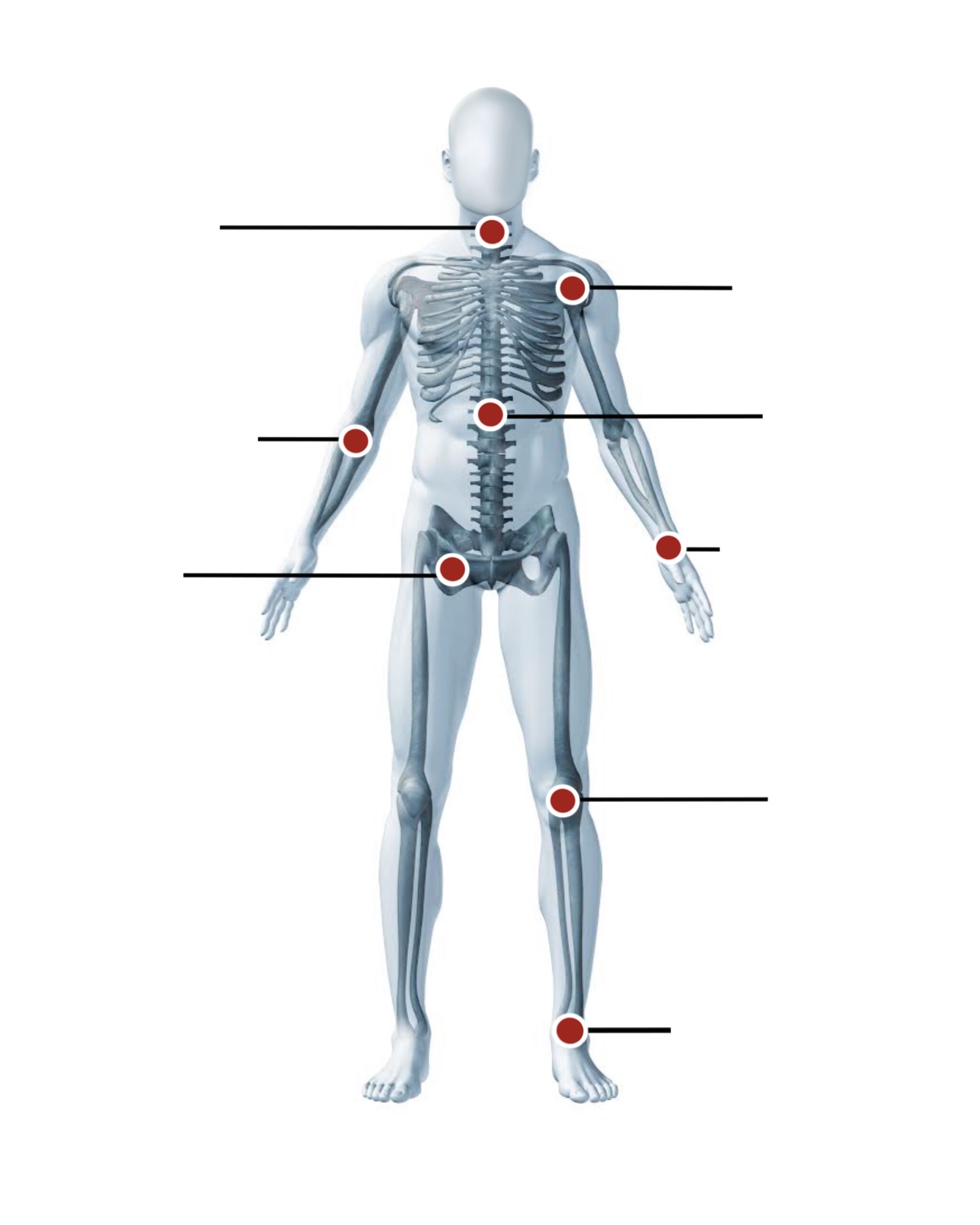
Neck
Shoulder
Elbow
Spine
Hand & Wrist
Knee
Foot & Ankle
Hip
See If We Are in Your Network
Questions?
The OPA team includes Alaska’s leading specialists and offers some of the latest, most advanced treatment procedures available today.
OPA treats a wide variety of conditions and offers comprehensive treatment options — including many non-surgical solutions, minimally invasive arthroscopies (repairs) and total joint replacement.